Julie Wasserman, MPH
Health Policy Consultant
TO: Green Mountain Care Board
RE: Comments on OneCare Vermont All Payer Model 2021 ACO Budget
FROM: Julie Wasserman, MPH
DATE: December 15, 2020
__________________________________________________________
Thank you for the opportunity to comment on OneCare’s 2021 Budget. The following comments focus on five critical areas: OneCare’s ACO Model, OneCare’s Financial Performance, Prospective Payment and Risk, Primary Care, and OneCare’s Quality Performance. In summary, OneCare is ill-suited to achieve widespread participation in the All Payer Model. OneCare’s financial performance is faltering, prospective payments are minimal and hospital risk is waning. OneCare’s primary care policy is counter-productive, and underlying quality performance problems persist. Recommendations accompany the conclusion.
OneCare’s ACO model
Population-wide health care reform is a deeply held Vermont principle. Proponents of the All Payer ACO Model emphasize that success will come only when there is widespread participation by Vermonters. Success will require “that all patients — and I really mean all — are under the model,” said Elliott Fisher, architect of the ACO and professor of health policy at the Dartmouth Institute. Until that happens, Vermont won’t “achieve the hoped-for gains.”
OneCare is ill-suited to achieve widespread participation in Vermont’s health care reform efforts due to ACO carve-outs and regulatory provisions. Lowering the thresholds to make it easier for OneCare to meet the federally required Scale Targets fails to address this critical problem.
The following groups of Vermonters are carved out or excluded from OneCare:
• Uninsured Vermonters. A recent Families USA report found 7% (28,000) of Vermonters were uninsured as of May 2020. These numbers may have grown due to the pandemic’s deepening economic recession. Addressing access to care for all Vermonters is a fundamental statutory tenet, supported by the lead sentence in AHS’s recent “reboot” report: “All Vermont residents should have access to high quality, affordable health care.” Nonetheless, the uninsured are excluded from OneCare.
• Newborns and children up to 1½ years old, some of whom may require neonatal intensive care or have serious childhood conditions. OneCare explicitly excludes these children in its Medicaid contract. Has OneCare employed this same exclusion in its BCBSVT contracts?
• Expenditures for Medicaid beneficiaries who have Medicare (Dually Eligible) are excluded from OneCare’s budget. AHS’s “reboot” recommends: “AHS, OneCare Vermont, and community providers should improve collaboration to strengthen integrated primary, specialty, and community-based care models for people with complex medical needs.” Medicaid beneficiaries who are Dually Eligible have some of the most challenging and complex medical needs in the entire Medicaid program. Why have their Medicaid expenditures been carved out of OneCare’s Medicaid budget?
• Individuals who obtain coverage after the start of the ACO Performance Year (January 1st). Individuals are excluded from OneCare if they enroll in Medicare, Medicaid or a commercial plan after the beginning of the Performance Year. There can be no additions to OneCare once the Performance Year has begun.
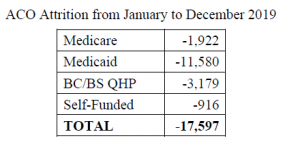
• Individuals attributed to the ACO whose insurance coverage changes or ends during the course of the Performance Year are removed from the ACO. More than 17,000 individuals were withdrawn from OneCare during the 2019 Performance Year:
• Vermonters participating in Medicare Advantage programs are ineligible to participate in the ACO. The most recent count of Vermont’s Medicare Advantage enrollees totaled 22,315 (CMS report). This is a growing population whose numbers have almost doubled since 2017. Note: Blue Cross/Blue Shield has just introduced its new 2021 Medicare Advantage Plan “Vermont Blue Advantage” whose participants will be excluded from OneCare.
• Alternative commercial insurance plans for Vermonters bypass the ACO. MVP has recently introduced its new 2021 Employer Level-Funded Health Plan which excludes members from OneCare.
• Innovative commercial options also sidestep the ACO. MVP has just initiated “Gia,” a digital front door addition to their commercial products that provides digital triage, telemedicine, and care concierge services 24/7 by phone, web, or mobile app.
OneCare’s ACO model will not achieve the stated and necessary All Payer Model goals and targets. In 2020, the 3rd year of the 5-year All Payer Model, OneCare served a minority of Vermonters (223,158). In 2021, only ≈ 238,000 people will participate in the ACO (an increase of only 15,000). Note: both the number of Medicaid ACO providers and the number of Medicaid attributed lives have decreased for 2021. OneCare’s administrative costs exceeded $40 million over the last 3 years (2018-2020), and cumulative administrative costs are projected to surpass $80 million over the course of the All Payer Model ACO initiative – see Appendix A. These substantial administrative costs are difficult to justify for so few Vermonters.
OneCare’s 2019 Financial Performance
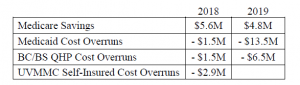
Honesty and transparency are vitally important in this age of misinformation. However, in a widely distributed October 2020 press release, OneCare claimed over $11 million in 2019 Medicare savings. The facts tell a different story. Of the $11.1 million in ACO “savings,” $6.3 million was pass-through money from CMS to assist with OneCare’s cash flow. This upfront money funds Blueprint and SASH and is recouped by CMS at the end of the year. The Green Mountain Care Board (GMCB) had the opportunity to publicly correct OneCare’s misrepresentation; however, they failed to do so. OneCare’s actual Medicare savings totaled $4.8 million, a fact that the GMCB neglected to clearly state at its recent hearing on OneCare’s 2019 financial results. The omission of this highly relevant finding from an impartial regulator is inexplicable.
ACOs are supposed to reduce the cost of care and produce savings. OneCare has largely done the opposite. (This is pre-COVID.)
OneCare’s financial losses and cost overruns have been a constant since its inception in 2014. The ACO’s cumulative cost overruns during the All Payer ACO Model initiative total roughly $26 million, offset by $12.8 million in savings – see Appendix B. Vermont is witnessing a downward trend in OneCare’s financial performance. OneCare’s Medicare savings have fallen from the prior year, and OneCare’s cost overruns in Medicaid and Blue Cross/Blue Shield have grown:
Given OneCare’s poor performance with Blue Cross/Blue Shield in both financial (above) and quality (below) domains, it is curious that the AHS “reboot” recommends greater OneCare/BCBSVT participation for State employees, teachers, and hospital employees.
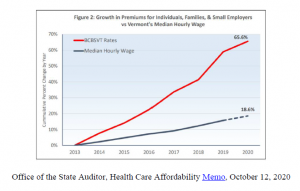
Legislators may be mistaken in their belief that having a private entity control Vermont’s health care system absolves the state of “risk.” In 2019, OneCare lost $20 million in Medicaid and Blue Cross/Blue Shield against savings of $4.8 million in Medicare for a net loss of $15.2 million. Add in OneCare’s administrative costs of $15.4 million and this program cost Vermont $30.6 million against budget. OneCare is not paying the difference; rate payers and taxpayers are. The cost of health care grows ever larger with OneCare’s cost overruns which we all subsidize through higher premiums, co-pays, deductibles, and rising school budgets. A notable uptick in the growth of commercial health insurance rates coincides with the implementation of the All Payer ACO Model (2018) – see below. Health care has become increasingly unaffordable for Vermonters.
Prospective Payment and Risk
OneCare’s prospective payments during the height of the COVID pandemic have been touted as saving the day; however, the real savior was the millions of dollars in Federal and State COVID stabilization funds received by hospitals. Vermont hospitals received over $365 million in federal COVID-related relief funds and almost $67 million in Vermont Provider Stabilization Grants (first application cycle) for a total of $432 million to date. OneCare’s prospective payments to the hospitals during the 3-4 intense COVID pandemic months pale in comparison.
OneCare’s prospective payments feature prominently as the hallmark of the All Payer Model. However, the GMCB has reported that the “ACO population and budget are a small subset of Vermont’s total population and spending” and show OneCare’s 2019 total cost of care as a mere 10% of Vermont’s total resident expenditures. Although proponents boast of OneCare’s success with prospective payment, “non fee-for-service spending currently comprises only 7% of Vermont’s health care spend.” (Quote from GMCB staff, Alena Berube, April 2020.) Prospective payments comprise only 14.5% of 2021 hospital budgets.
Provider “risk” constitutes the central pillar of the All Payer ACO Model. Risk-based arrangements tied to healthcare expenditures constitute the financial construct of the ACO. However, OneCare has all but abandoned risk. OneCare’s 2019 and 2020 contracts with Blue Cross/Blue Shield required risk of 6%, yet risk was abandoned. Blue Cross/Blue Shield bore no risk in 2019 and 2020, and will bear none in 2021. Medicaid and Medicare risk for hospital payments in 2019 and 2020 were 4% and 5% respectively; however, these risk corridors have dropped to a mere 2% in 2021
(and 1% for Medicaid Expanded), implying the ACO wants to further minimize its responsibility for cost overruns. The AHS reboot recommends reducing Medicare risk even further to 1.5% to foster greater hospital ACO participation. Hence, OneCare is evolving toward a non risk-based model for the most expensive sectors of health care. This raises questions about the value of the ACO. To further compound this problem, OneCare has cut upfront reimbursements for primary care physicians, insisting they can earn it back at the end of the year if the ACO meets its performance goals. In so doing, OneCare has put primary care physicians at financial risk for the ACO’s overall performance over which they have little control. Consequently, OneCare’s 2021 risk initiatives put primary care physicians at risk while essentially instituting a no risk strategy for hospitals. This constitutes upside down policy making, given that primary care physicians make up less than 10% of health care expenditures while hospitals comprise almost 50%.
Primary Care
Fay Homan MD, a Vermont family physician, states in her Digger Commentary, “Any approach to increasing quality and decreasing cost is built on a strong foundation of primary care. However, there simply aren’t enough primary care providers in Vermont now, and the number is decreasing at an alarming rate. Strategies – effective ones – exist to avert this crisis. The problem is that we are not implementing them in a significant or systematized way.” Rather than allowing OneCare to weaken primary care, the State should instead implement the following initiatives to strengthen and fortify primary care.
• Rescind OneCare’s new reimbursement arrangement with primary care physicians that significantly reduces their guaranteed upfront payments.
• Increase compensation for primary care physicians. The Agency of Human Services
concurs, stating at a recent GMCB Primary Care Advisory Group meeting that prioritizing primary care provider reimbursements is a priority of the All Payer Model.
• Institute loan forgiveness and debt reduction programs.
• Reduce administrative burdens and “productivity” metrics.
• Offer free tuition to UVM medical students who pledge to practice primary care in an underserved area of Vermont.
• Increase the number of UVM Medical Center residency positions in primary care.
• Coordinate with UVM Medical Center’s primary care residency programs (family
practice, internal medicine, pediatrics) to implement creative initiatives to attract out-of-state physicians.
• Listen to primary care physicians, many of whom voiced concerns at a recent GMCB
meeting about OneCare’s payment cuts, Care Navigator, OneCare’s data redundancies, confusion over OneCare’s quality metrics, OneCare’s clinical relevance, the lack of meaningful patient resources, workforce issues, payment inequities between specialists and primary care physicians, unpredictable and inadequate compensation, patient affordability issues, and the growing number of uninsured.
OneCare’s 2019 Quality Performance
OneCare’s high Quality Performance scores for Medicare (92%) and Medicaid (95%) camouflage some troubling trends. Additionally, OneCare’s quality performance with Blue Cross/Blue Shield has worsened.
Medicare
Reducing avoidable hospital readmissions is a critical indicator of quality, especially for the Medicare elderly who fare poorly when hospitalized. OneCare’s poor performance with avoidable hospital readmissions is evidenced by the following two measures. [Percentile categories range from 30% (lowest) to 90% (highest)].
• Risk-Standardized, All Condition Readmissions
(OneCare scored in the 50th percentile; worse than the prior year.)
• All-Cause Unplanned Admissions for Patients with Multiple Chronic Conditions
(OneCare scored in the 40th percentile)
Medicaid
• Hypertension: Controlling High Blood Pressure
This is one of the most important population health indices. Yet OneCare’s 2019 score (62.63%) is lower than 2018 (63.9%) and even lower than 2017 (64.61%). This represents a 3-year downward trajectory on a crucial population health measure.
• Initiation of Alcohol and Other Drug Dependence Treatment
OneCare’s 2019 score remains in the 25th percentile (lowest), having been there for two consecutive years (2018, 2019), and having been below the 25th percentile in 2017. This weak performance is cause for concern given the All Payer Model’s primary goal of reducing suicides and drug overdose deaths, not to mention Vermont’s opioid crisis.
Blue Cross/Blue Shield
OneCare’s overall Blue Cross/Blue Shield quality score has worsened in 2019 – see table below. Of the nine ACO quality measures, performance in more than half (5) declined from the prior year. Initiation and Engagement of Alcohol and Other Drug Dependence Treatment is one of the worsening measures and it sits in the 25th percentile (lowest). Blue Cross/Blue Shield concedes it is difficult to determine the impact of the ACO’s quality initiatives on its members.
ACO Year BC/BS
QHP Quality Score
2017 73.07%
2018 86.12%
2019 80.56%
Conclusion
OneCare is ill-suited to achieve widespread participation in Vermont’s health care reform efforts. OneCare’s overall financial performance is poor, prospective payments are insubstantial and hospital risk is diminishing. OneCare’s primary care policies do not strengthen the primary care provider workforce, and underlying quality performance problems remain.
Recommendations
1. The GMCB needs to consider alternative models of health care reform that allow for widespread participation of Vermonters.
2. The GMCB needs to conduct an analysis of OneCare’s 2019 financial results and the underlying methodologies to determine why OneCare generated $4.8 million in Medicare savings while simultaneously incurring losses of $20 million in Medicaid and Blue Cross/Blue Shield. (Was the Medicare cap on spending set high?) What did OneCare do differently for the populations? If the same basic services were offered, how does OneCare explain the difference in results? Physicians do not alter their practice patterns based on a patient’s insurance coverage.
3. The All Payer ACO Model Agreement contains three high level population health goals, one of which is to increase access to primary care. Implementation of the aforementioned primary care initiatives would address this goal.
4. The GMCB needs to question whether Vermont needs an ACO to implement prospective payments and other “predictable” payment mechanisms. (Where is the predictability in OneCare’s $13.5 million Medicaid overspend?) DVHA is well-versed in prospective payment and value-based models, possessing considerable expertise in implementing such programs (Children’s and Adult Mental Health, Residential Substance Use Disorder Program, and Developmental Disabilities Services, among others). Moving ACO functions into state government may be a prudent approach to controlling health care expenditures, implementing payment reform, improving quality and care management, and integrating services. Additionally, the state could consider hospital global budgets, and rate-setting as outlined in Act 48.
5. An independent evaluation of OneCare’s effectiveness in Vermont’s health care reform efforts needs to occur prior to making a decision on a second 5-year renewal of the All Payer ACO Model Agreement.